Let me start by saying the topic of Diminished Ovarian Reserve or Premature Ovarian Failure, although the conventional description of this topic, are not terms I like to use.
With premature ovarian failure, there is no failure. No one has done anything wrong. It is not your fault. However, since this is a common term that everyone knows, I will refer to it to provide context.
To provide understanding on the discussion of Diminished Ovarian Reserve (DOR) I will give you context by covering:
- Ovaries: How They Work
- How to contend with what is happening, over time, with your ovaries
- What is Diminished Ovarian Reserve (DOR)
- What Causes Diminished Ovarian Reserve
- DOR: What are the Treatments?
How Do Ovaries Work?
When it comes to the quantity and quality of eggs, women are on a continuum, and at varying points, something can happen. Sometimes their ability to conceive can be bad, and at another point can change to be good again. Women can go from having very few eggs to all of a sudden having more eggs.
This is particularly true with autoimmune sources, as noted from the American College for the Advancement in Medicine, “It is known that autoimmune diseases such as diabetes, autoimmune thyroiditis and systemic lupus erythematosis are linked to decreased fertility. Other causes of infertility such as premature ovarian insufficiency, endometriosis and polycystic ovarian syndrome include autoimmune components.”
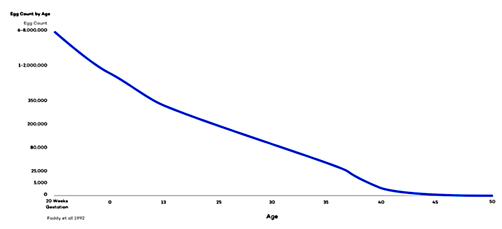
Below is a picture of where the eggs are as they start off at birth and their progression over time.
How many eggs are female humans born with?
As a fetus early in development, a female has around a whopping 6 million eggs. The number of these eggs (oocytes, to be precise) is steadily reduced so that when a baby girl is born, she has between 1 and 2 million eggs. (Sources differ slightly, but regardless, we’re talking about a seven-digit figure!)
So why doesn’t the menstrual cycle start at birth?
Good question. The eggs are there, so what’s stopping the menstrual cycle from starting up? The menstrual cycle is on hold until a girl reaches puberty. Puberty begins when the hypothalamus in the brain starts to produce gonadotropin-releasing hormone (GnRH). In turn, GnRH stimulates the pituitary gland to produce follicle-stimulating hormone (FSH). FSH initiates egg development and causes estrogen levels to rise
How many eggs does a girl have when she reaches puberty?
When a girl reaches puberty, she has between 300,000 and 400,000 eggs. Hey, what happened to the rest of those eggs? Here’s the answer: Before puberty, more than 10,000 die each month
https://www.healthline.com/health/womens-health/how-many-eggs-does-a-woman-have#how-many
You will see that over time as you get to your late 30s, there are far fewer eggs. Everyone thinks, ‘oh, my gosh, I’m hitting my 30s. I’m really losing all my eggs now.”
Medically speaking, you can say that a person has actually been losing eggs since birth. And really, it’s just as you start hitting the late 30s and early 40s where there’s far less egg reserve left and so, it starts to matter more.
What are antral follicles and what that means for egg retrieval.
Antral follicles are small egg-containing follicles (about 2–9 mm in diameter) that can be seen, measured and counted with ultrasound. They’re also referred to as “resting” follicles because they’re the ones that are primed to grow, ready for ovulation, in this particular menstrual cycle. Antra Follicles host immature eggs until they are ready to be released.
Low antral follicle count can contribute to difficulties in getting pregnant, but this does not mean it will be impossible to conceive. I have seen patients with low Antral Follicle Count (these are the small egg-containing follicles that can be seen, measured, and counted with ultrasound.
Antral Follicles are also referred to as “resting” follicles because they are the follicles that are primed to grow and ready for ovulation) where we have gotten six or even ten blastocysts. This isn’t to say that there isn’t a good egg in the midst, but it means these people were struggling for years with a ton of eggs where they were trying to get sperm and egg to meet each other, but the DNA inherent to the egg had mistakes.
Similarly, I have seen people where we’ve gotten six or even ten blastocysts, and where almost all of them were chromosomally abnormal. This isn’t to say that there isn’t a good egg in the midst, but it means these people were struggling for years with a ton of eggs where they were trying to get sperm and egg to meet each other, but the DNA inherent to the egg had “mistakes.”
What is the Production Line Theory?
This is one of the dogmas that we teach to every single med student, called the Production Line Theory.
The Production Line Theory posits that the last oocytes in the ovary are intrinsically less healthy and represent the last oocytes released by the ovary. This theory suggests that quantity and quality decline in parallel. ASRM.
The Production Line Theory is based on the fact that all the eggs you’re born with are the ones you have for life. But the eggs that you ovulate later in life are essentially later generation copies and so they are more likely to make “mistakes.”
And so, this interaction on the continuum, as the quantity of eggs goes down later in life and the rate of chromosomal abnormalities increases, impacts your fertility chances.
This is one of the hard things to explain about Ovarian Reserve Counseling. Although, some people do not have as many eggs, they can still have fewer eggs with very good quality.
My wife was running out of eggs when we had our son Lucus at age 41. But we were blessed with a baby boy that in our book is pretty high quality and a good kid! And so, I’m very happy with the outcome 🙂
DOR: What is it?
Ultimately, I prefer Diminished Ovarian Reserve (DOR) versus Premature Ovarian Failure – which describes a point when the ovaries stop functioning normally before age 40 When this happens, your ovaries don’t produce normal amounts of the hormone estrogen or release eggs regularly and there is often no ability to get pregnant. But with DOR that is really not entirely the case.
According to the American Society for Reproductive Medicine, “The ovarian reserve refers to a woman’s fertility potential in the absence of any problems in the reproductive tract (fallopian tubes, uterus, vagina). It mainly depends on the number and quality of eggs in the ovaries and how well the ovarian follicles are responding to the hormonal signals from the brain.” https://www.asrm.org/topics/topics-index/ovarian-reserve/
When it comes to the quantity and quality of eggs, women are on a continuum, and at varying points, something can happen. Sometimes their ability to conceive can be bad, and at another point can change to be good again. And so you can go from having very few eggs to all of a sudden having more eggs.
What Causes DOR?
It is not just a quantity issue, but a quality issue.
Generally, as you age the number of quality eggs you hare in reserve diminish.
- When you are in your 20s, 80-90% of eggs are chromosomally normal.
- As you get into the early 30s, maybe 2/3rds are good.
- And as you get to mid to late 30s, roughly 1/3rd are good quality.
- Certainly, by the 40s, it’s reduced to a quarter or less.
- By 45, you can even see 90-95% of eggs are chromosomally abnormal.
This is one of the most important aspects in calculating quantity vs quality. The more eggs have available the more likely there is a good one in there. Also, the older we get the more likely there is a quality issue. And so if you’re 45 and you have one egg to choose from in a month and 90-95% are abnormal, it might mean you only release one high quality egg per year, which makes it really hard to get pregnant downstream.
And there are just fewer opportunities to conceive compared to a person who is 30 years old, where they may get three eggs and most of them are normal.
How Age Factors into Fertility.
We realize that people often worry only about advanced maternal age — like “I’m 38, and I cannot have a child.” It is not that simple. You can be older, but the real question is the status of your baseline reserve for your eggs. Often, in the fertility process, women can overcome little mistakes in egg quality and still get pregnant.
Think of your fertility journey like a book.
You can have a book and if it is missing a chapter or missing a page, that is pretty severe. And a lot of people would say, hey, there is something meaningfully wrong with this book.
Conversely, if you have an extra word or are missing a word, or an extra letter or are missing a letter, those are usually small enough not to be noticed.
And this is the same with conception because when eggs or embryos don’t work the way they should and it’s invisible, it’s because of those “missing words or letters” that are still too small to be picked up with conventional testing.
As you age, a higher percentage of the eggs inside your ovaries contain these missing “words or letters” called genetic abnormalities. The eggs inside your ovaries are “primordial,” or immature eggs. As you ovulate, they go through another phase of cell division, known as meiosis. Older eggs are more likely to accumulate errors in their DNA during that division process, leading to genetically abnormal eggs.
Lifestyle and Autoimmune Diseases: The Impact on the DOR Fertility Journey
Let’s understand some of the variations that can cause changes in your fertility levels. When you go back to the graph showing the diminishing number of eggs from birth, research shows there are some women you have about as many eggs in the bottom 5% as women who are in the top 5% at age 40. This is where some of the variations happen.
Here are three such factors that can impact your reproductive outcomes.
- A medical event can impact reproductive outcomes. You can be going along the curve, cruising along, and then all of a sudden, boom, it drops down where a sudden medical event changes everything, i.e. chemotherapy, radiation, or surgery that removes part of your ovary. And suddenly, your ovarian reserve completely changes, but you continue on the lower trajectory.
- Autoimmune diseases: inflammation caused by autoimmune diseases such as diabetes, autoimmune thyroiditis, and systemic lupus erythematosus (SLE, a chronic disease that causes inflammation in connective tissues) are linked to decreased fertility where they look older than their biological age.
- And you can see this with lifestyle factors that can impact reproductive health such as nutrition, weight, exercise, psychological stress, environmental and occupational exposures, cigarette smoking, illicit drug use, and alcohol and caffeine consumption can negatively influence fertility.
According to reproductivefacts.org, “chemicals (such as nicotine, cyanide, and carbon monoxide) in cigarette smoke speed up the loss rate of eggs. Unfortunately, once eggs die off, they cannot regenerate or be replaced. This means that menopause occurs 1 to 4 years earlier in women who smoke (compared with non-smokers).” https://www.reproductivefacts.org/news-and-publications/patient-fact-sheets-and-booklets/documents/fact-sheets-and-info-booklets/smoking-and-infertility/
For context, that roughly means, if you smoke:
- a quarter pack a day, your ovaries are about a year older
- half pack, two years older
- and a pack a day, three years older
The amount and length of time of smoking matters because it is bad for getting pregnant, and some argue can drop your fertility by roughly 40%. But some people think that if you stop smoking, they are in the clear.
The reality is, if you have been smoking long enough, it takes a long term hit for your ovaries. So, if you are 28 but your ovaries are now 31 by aging three years from long term smoking, of course, you can still get pregnant? But if you are 38 and your ovaries have aged 3 years to 41, that’s a meaningful hit for ovarian reserve, and that makes it very hard to conceive.
So, what we want to be mindful of are factors within our control. We cannot control autoimmune disease or prevent the inflammatory environment we were brought up in, like secondhand smoke. But we want to minimize inflammatory environments we are in control of, and practicing good health and well is a good thing.
If you want to learn more, go to an article written by the American Society for Reproductive Medicine called “Smoking and infertility: a committee opinion.” https://www.asrm.org/globalassets/asrm/asrm-content/news-and-publications/practice-guidelines/for-non-members/smoking_and_infertility.pdf
Diagnosing DOR
PGS involves testing an embryo for chromosomal abnormalities. Many embryos with chromosomal abnormalities will not lead to a pregnancy or will result in a miscarriage. All women will have some eggs that are chromosomally abnormal. All men will have some sperm that are chromosomally abnormal. The percentage of embryos that are abnormal can be affected by many factors, including the age and health history of the parents.
As a rule, I do not like to do preimplantation genetic testing PGT early on, particularly when there’s diminished ovarian reserve. Because although if you do testing, you can identify Down syndrome and can identify quality issues for the eggs.
The challenge is if you do IVF and you get three eggs and end up with one blastocyst and one high quality embryo, you’re now adding $3,000 – 4000 to the cost of PGT to diagnose the quality of just the one embryo that would either take or not, so it’s not helping you. You are stuck with the one you’ve got, and that’s one of the key challenges
What does this mean? It means that it is much better in the IVF process if I harvest 10 embryos and among them we see there are five normal and five abnormal, so we can just put one of the normal ones back.
The trick is we must work to get as many eggs as we can for quantity and manage the quality.
The Options for Treating DOR
Understanding the journey is important in terms of managing the expectations for people. Many times, when you completely run out of eggs, you are usually looking at about a 5-10% lifetime chance of bringing home a baby on your own using your own eggs.
There seems to be a slightly higher percentage if you are in your younger 20s or for someone with autoimmune disease because of how those diseases can wax and wane. The autoimmune disease can be there and then disappear and then the eggs show up again. But for a lot of people experiencing long-standing infertility or they are older, or they have fewer eggs left, they are more likely to be abnormal. This makes for very slim chances and it can be very painful for the patient.
#1. Of course, you can start younger but that is after the fact and you cannot really fix that.
#2. You can get more eggs. revving up the eggs that are there If you have three eggs in a month, that is triple the chance of finding a normal one relative to just one.
#3. Doing insemination to improve the chances a sperm can find the egg
#4. Use eggs from someone else via an egg donor. With donor eggs, you would carry the pregnancy even if the eggs do not contain your DNA.
I had a patient who recently said “I am never going to use a donor egg because I am not paying for me to carry a pregnancy that my husband had with another woman” Although I can empathize with where she’s coming from, that is not how the biology works.
Remember that when you are carrying the pregnancy, there are Epigenetic Influences.
The way to think of that is that if there is an electrician that wires your house, you are still determining which light switches are on and off. While some of that is inherent to the wiring, the other is from what activates within your body. You can find all these instances where a child looks so much like the woman who carried them and delivered them, even though it was not her DNA.
This is not even considering the other aspects child development such as love and support from the first moment, the ability to breastfeed, and the ability to avoid toxins during pregnancy. Some people also feel that if they use someone else’s eggs with their partner’s sperm, and they carry the pregnancy, that can give some control back to the process.
I think we must think about what is right for people. And in terms of exploring what happens for the eggs, you can only use the eggs you have. You can try to rev them up so that sperm are more likely to find them. You can even do embryo culture through IVF, where you have better chances per egg by being outside of the body initially. You can reduce endometriosis as you reduce pelvic inflammation and make the uterus as hospitable as possible.
Ultimately, there is no surgery that we have currently that meaningfully changes the DNA inherent to an egg. And you just simply must play the hand that you have been dealt for where those eggs are. There are a lot of conversations around ovarian rejuvenation and using stem cells to replenish the eggs, but I have not seen the data to say it is ready for prime time. I cannot wait until we can get there, but I think a lot of people are holding out hope and holding their breath for something that, technologically, is not ready or available quite yet.
If you are wanting to build your family, we would love to help you. From simple explanations to high tech solutions, or a simply a fresh perspective if what you’ve been doing on your own or with a doctor hasn’t worked, come see us in our Monroe, Shreveport, Madison, Starkville, or Hattiesburg MS offices.
Call us at 833-767-7837 and let’s help you have the child of your dreams!
J. Preston “Pres” Parry, MD, MPH




