Female Fertility Testing
What Causes Infertility in Women?
Three key factors impact female reproduction.
#1 Causes of Female Infertility | Viable Eggs
- Generally speaking, in your 20s, 80-90% of eggs are chromosomally normal.
- As you get into the early 30s, maybe 2/3rds of eggs are healthy
- As you age to your mid to late 30s, roughly1/3rd of eggs may be of good quality.
- And by the time your reach your 40s, your quality egg reserve may be reduced to a quarter or less.
- By 45, you can even see 90-95% of eggs are chromosomally abnormal.
So, when looking at the eggs, this is one of the most critical aspects in calculating quantity versus quality. The more eggs you have available in the fertility continuum, the more likely there is a good one to initiate a pregnancy. In contrast, the older we get, the more likely an egg quality issue will be present as we age. Translation: Ovarian reserve diminishes with age, making pregnancy less likely. So, if you’re 45 and have one egg to choose from in a month and of your fewer egg reserve, 90-95% are chromosomally abnormal, it might mean you only release one high-quality egg per year, which makes it harder to get pregnant downstream. When measuring ovarian reserve, the objective is to determine whether you can release a sufficient number of healthy eggs into the fallopian tubes. 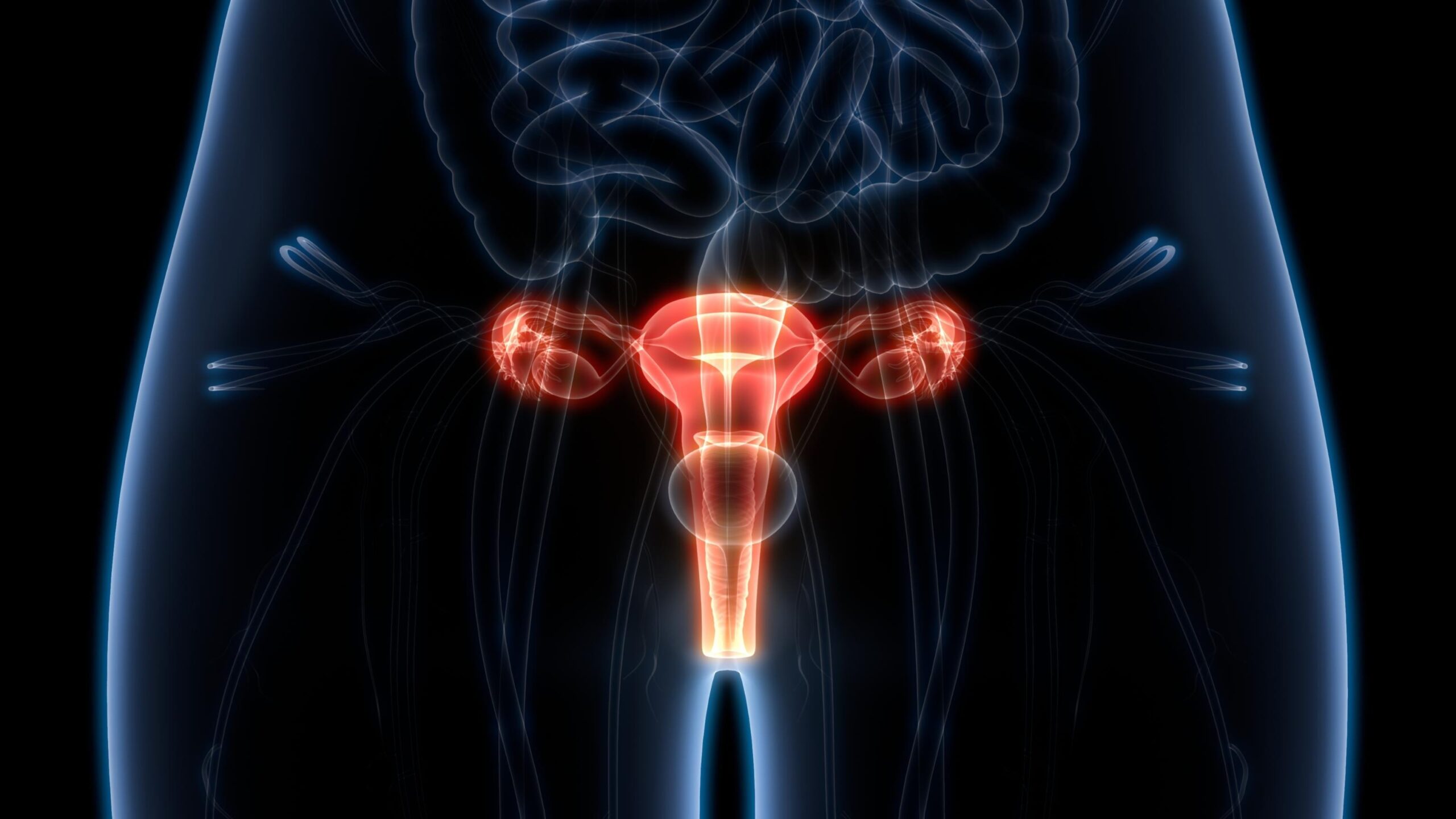
Ovarian Reserve Fertility Testing
Measuring ovarian reserve is a two-pronged approach involving lab work and ultrasound imaging for AFC (antral follicle count) testing (which we prefer). Some of the more common lab tests are FSH, E2, and AMH, all of which are discussed below. Evaluation typically measures the number of ovarian egg sacs -called follicles – or hormonal shifts reflecting egg quantity. Of note, beyond estimating through age, there are no great tests for egg quality outside IVF itself (including PGT-A where one looks at the DNA) and pregnancy.
AFC Testing – Antral Follicle Count
AFC testing is a simple count of mature follicles in the ovaries. It is done via transvaginal ultrasound, enabling a fertility specialist to view an enlarged image of the reproductive system and count the number of follicles by sight. An AFC count can reveal whether the number of eggs is consistent with that expected for one’s age. It can also serve as an indicator of whether IVF will produce desired results. However, though AFC and AMH are considered the gold standards, neither are perfect.
FSH – Follicle-Stimulating Hormone Test (FSH)
“The FSH test measures the level of follicle-stimulating https://medlineplus.gov/hormones.html (FSH) in your blood. FSH is made by your pituitary gland, a small gland located underneath the brain. FSH plays an important role in sexual development and functioning.” In women, FSH tests are most often used to:
- Help find the cause of infertility.
- Find out if there is a problem with ovarian function .
- Find the reason for irregular or stopped menstrual periods.
- Confirm the start of menopause or perimenopause. Menopause is the time in a woman’s life when her menstrual periods have stopped, and she can’t become pregnant anymore. It usually starts when a woman is around 50 years old. Perimenopause is the transition period before menopause. It can last for several years. FSH testing may be done towards the end of this transition.”
A blood sample was drawn on cycle day three to measure follicle-stimulating hormone (FSH) levels. The primary role of FSH is to ensure egg growth within the follicle so that mature eggs are released during ovulation. Of note, FSH is a late marker of ovarian problems, where only 50% of women over age 45 will have elevated FSH.
E2 estradiol test
An E2 test measures estradiol levels in the blood. Estradiol (E2) is a form of estrogen produced by the ovaries. A woman’s E2 count needs to be within a specific range. When it is too high, E2 suppresses FSH levels, making conception difficult. When the count is too low, it’s often indicative of polycystic ovary syndrome , which also inhibits fertility. Estradiol levels can affect how the reproductive system develops. Abnormally high or low levels can influence how the following parts of the body grow and work:
- womb
- fallopian tubes
- vagina
- breasts
- libido
- erectile function
- sperm cells
During their reproductive years, women usually have their highest levels of estradiol. After reaching menopause, estradiol levels are much lower. Unfortunately, because estradiol levels fluctuate over the menstrual cycle, this is a very low-reliability test, where AFC and AMH are much better.
AMH Anti-Müllerian Hormone Test
Ovarian follicles produce a hormone called AMH. AMH serves a number of roles, but perhaps the most important is sex differentiation between male and female embryos. It keeps baby boys in the womb from developing girl parts and vice-versa. Essentially, though, the higher your AMH levels, the higher your ovarian reserve because a high AMH count indicates a greater number of follicles in the ovaries. “An AMH test is often used to check a woman’s ability to produce eggs that can be fertilized for pregnancy. A woman’s ovaries can make thousands of eggs during her childbearing years. The number declines as a woman gets older. AMH levels help show how many potential egg cells a woman has left — known as the ovarian reserve. If a woman’s ovarian reserve is high, she may have a better chance of getting pregnant. She may also be able to wait months or years before trying to get pregnant. If the ovarian reserve is low, it may mean a woman will have trouble getting pregnant, and should not delay very long before trying to have a baby.”
Inhibin B Hormone Test
Inhibin B testing can be used in cases where there is an unexpected poor response to the stimulatory medication or in women who have unexplained infertility. Some centers use it for all of their egg donors to optimize their donor pool. In rare instances, a clinic may order testing for Inhibin B. As their name suggests, these are inhibitor hormones, and they both play a role in suppressing FSH, the hormone that stimulates egg growth. Inhibin B is a hormone that is produced by certain cells in the ovarian follicles. When produced, it helps to suppress another hormone called FSH, or follicle-stimulating hormone. FSH is secreted by the brain and causes an egg follicle to grow on the ovary. As a woman ages, not only does the number of follicles on the ovaries decrease but so do the hormones produced by those follicles, like inhibin B. Unfortunately, this test, like estradiol and FSH, is a less reliable marker than AFC and AMH
#2 Causes of Female Infertility | Fallopian Tubes
Hysterosalpingogram HSG Testing
According to the American College of Obstetricians and Gynecologists, “Hysterosalpingography (HSG) is an X-ray procedure that is used to view the inside of the uterus and fallopian tubes. It often is used to see if the fallopian tubes are partly or fully blocked. It also can show if the inside of the uterus is of normal size and shape. All of these problems can lead to infertility and pregnancy problems.” Though HSGs have been performed on women for over 100 years, it is arguable how much that test has advanced over that time. An HSG involves using a catheter, which is inserted into the cervix through the vagina. An iodine liquid is then sent through the catheter, outlining the length of the fallopian tubes. Finally, X-rays of the reproductive system are taken, the iodine causing the fallopian tubes to show up on the resulting film. During the procedure it is not uncommon for women to experience cramping and discomfort. Cramping and vaginal spotting or bleeding may be experience for 24 to 72 hours after the procedure. HSG testing can pose a risk of allergic reaction to the dye solution, potential infection and damage to pelvic structures from the instruments used.
An Alternative to HSG Fertility Testing
 Dr. Parry has cared for many women through his career and has performed thousands of fertility tests. But through his experience, he found many combinations of fertility tests used today to identify infertility in women – typically including blood tests, physical examinations, biopsies and special imaging procedures – to be inaccurate, painful, and the results to be confusing for his patients. Dr. Parry went to work to develop the patented Parryscope® technique, a gentle (radiation-free) alternative to hysterosalpingogram (HSG) testing, that also works to identify obstructions in the fallopian tubes. Dr. Parry then took this fertility diagnostic approach a step further to develop the Parryscope approach, a single office test that can gently evaluate all at one time:
Dr. Parry has cared for many women through his career and has performed thousands of fertility tests. But through his experience, he found many combinations of fertility tests used today to identify infertility in women – typically including blood tests, physical examinations, biopsies and special imaging procedures – to be inaccurate, painful, and the results to be confusing for his patients. Dr. Parry went to work to develop the patented Parryscope® technique, a gentle (radiation-free) alternative to hysterosalpingogram (HSG) testing, that also works to identify obstructions in the fallopian tubes. Dr. Parry then took this fertility diagnostic approach a step further to develop the Parryscope approach, a single office test that can gently evaluate all at one time:
- the health of the ovaries
- the number of eggs remaining,
- whether there are any blockages in the fallopian tubes, and
- the condition of the uterus.
The procedure itself takes about 20 minutes. Then Dr. Parry takes great care in explaining the procedure, the results, and the next best step in treating infertility. The Parryscope Fertility Diagnostic approach is an alternative fertility testing method that presents less discomfort and fewer risks to women compared with many contemporary fertility testing and diagnostic approaches, including HSG testing. Related Information: Learn More About Parryscope
# 3 Causes of Female Infertility | What is the Uterine Factor
Transvaginal Ultrasound Fertility Test
The assessment of the uterine cavity in patients with infertility is essential as many intrauterine lesions can be detected. Transvaginal ultrasound (TVE) is a front-line test for female infertility. It allows assessment of the uterine cavity for detection of abnormalities responsible for fertility disorder as well as of lesions that may lead to transfer or implantation failures.  With transvaginal ultrasonography, as it is called, a small ultrasound transducer is inserted a few inches into the vagina, allowing us to see the reproductive system. For most, the procedure may cause some minimal discomfort, but it is completely safe and should not result in actual pain. The resulting scans can help physicians identify a number of conditions that may impede pregnancy.
With transvaginal ultrasonography, as it is called, a small ultrasound transducer is inserted a few inches into the vagina, allowing us to see the reproductive system. For most, the procedure may cause some minimal discomfort, but it is completely safe and should not result in actual pain. The resulting scans can help physicians identify a number of conditions that may impede pregnancy.
- Uterine scarring
- Internal bleeding
- An abnormal uterine shape
- Abnormalities in the uterine lining
- Cysts, fibroids, and other growths
- Pelvic inflammatory disease
- Endometriosis – a disorder where the tissue that’s supposed to line the interior of the uterus actually grows outside of it
- Of note, ultrasound often can miss disease within the uterus. Though saline-infused sonography and 3D ultrasound are better, there still sometimes can be difficulties with smaller pathology that are easily seen with hysteroscopy.
Hysteroscopy for Fertility Testing There is a limit to the resolution one can get with a 2D black and white image. Though 3D can improve this, there are some meaningful advantages where one intuitively recognizes problems with the use of live video looking inside the uterus. We find combining ultrasound with office hysteroscopy gives us our best blend of being accurate, thorough, gentle, and affordable. Moreover, we routinely find problems that other clinicians have missed when using this approach.
Pelvic sonogram
Also known as vaginal ultrasound, this procedure uses sound waves to help doctors visualize soft pelvic tissue such as the wall & lining of the uterus that cannot be seen using an x-ray. Pelvic sonograms are used to see, count and measure antral follicles. These small follicles, about 2 to 10 mm in diameter, hold immature eggs that have the potential to develop in the future. The antral follicle count (AFC), or number of follicles, is used to help doctors determine how many potential healthy eggs a woman has on reserve and the best treatment option for the patient. Pelvic sonograms can also identify uterine fibroids, noncancerous growths in the muscle tissue of the uterus that can sometimes impair blood flow, block the fallopian tubes and affect the overall health of the uterus. The Parryscope technique also performs the test function of a pelvic sonogram.
Saline infusion sonohysterogram
SIS, also called saline infusion ultrasound, is a procedure that evaluates the uterine tissue. During SIS the doctor will insert a saline solution into the uterus to improve the clarity of the ultrasound. This allows the doctor to assess the endometrium (lining of the uterus) to see if there is any scarring, if the lining has thickened or if there are any polyps (small generally noncancerous growths). Parryscope testing also uses a form of saline infusion for visualizing the uterus. Sometimes doctors will perform sonosalpingography (also known as HyCoSy for hysterosalpingo-contrast-sonography) to assess the fallopian tubes. This is a technique that not many physicians can perform, and they often have to have done quite a few to be good at it. Moreover, it can sometimes only see one fallopian tube instead of both, and many studies show it results in pain comparable to HSG.