A Breakthrough in Fertility Testing
When should you seek advice from a fertility specialist?
Our experience shows if you go a year with unprotected intercourse and are not successfully conceiving, the odds are about 5-to-1 against getting pregnant over the next several years of conceiving spontaneously.
If it’s been a year or longer and you haven’t been able to conceive, you should seek medical counseling.
What is the best approach to diagnosing infertility?
A fundamental question to fertility is often, what is the best approach to diagnosing infertility in women?
Diagnosing infertility depends on what is the source of the problem. If you don't know what it is, it's hard to fix. You have to have the proper testing before you decide on the right treatment.
Effective infertility testing, starts with understanding the right answers to your questions.
-
Are there sperm?
-
What is the quantity and quality of eggs?
-
Are the fallopian tubes open?
-
And is there a receptive place for the embryo in the uterus?
The answers to these questions guide effective treatment.
What tests are used for diagnosing infertility?
What are the common tests performed to diagnose infertility?
Fertility testing for women generally focuses on the following three factors affecting female reproduction: ovaries; fallopian tubes; the uterus.
Any evaluation for infertility should be done in a focused and cost-effective way to find all relevant factors and include the male and female partners.
The following tests may be recommended as part of your infertility evaluation:
Male Partner Semen Analysis
Although the semen analysis is obtained from the male partner, it is an essential part of the infertility evaluation. A semen analysis should provide information about the number, movement, and shape of the sperm. A semen analysis is necessary even if the male partner has fathered a child before.
Hysterosalpingogram (HSG)
This is an X-ray procedure to see if the fallopian tubes are open and to if the shape of the uterine cavity is normal. A catheter is inserted into the opening of the cervix through the vagina. A liquid containing iodine (contrast) is injected through the catheter. The contrast fills the uterus and enters the tubes, outlining the length of the tubes, and spills out their ends if they are open.
Transvaginal Ultrasonography
An ultrasound probe placed in the vagina allows the clinician to check the uterus and ovaries for abnormalities such as fibroids and ovarian cysts.
Ovarian Reserve Testing
When attempting to test for a woman’s ovarian reserve, the clinician is trying to predict whether she can produce an egg or eggs of good quality and how well her ovaries are responding to the hormonal signals from her brain. The most common test to evaluate ovarian reserve is a blood test for follicle-stimulating hormone (FSH) drawn on cycle day 3. In addition to the FSH level, your physician may recommend other blood tests, such as estradiol, antimüllerian hormone (AMH), and/or inhibin-B, as well as a transvaginal ultrasound to do an antral follicle count (the number of follicles or egg sacs seen during the early part of a menstrual cycle).Other Blood Tests:
Thyroid-stimulating hormone (TSH) and prolactin
TSH levels are useful to identify thyroid disorders and hyperprolactinemia, which may cause problems with fertility, menstrual irregularities, and repeated miscarriages.In women who are thought to have an increase in hirsutism (including hair on the face and/or down the middle of the chest or abdomen), blood tests for dehydroepiandrosterone sulfate (DHEAS), 17-α hydroxyprogesterone, and total testosterone should be considered. A blood progesterone level drawn in the second half of the menstrual cycle can help document whether ovulation has occurred.
Urinary Luteinizing Hormone (LH)
Over-the-counter “ovulation predictor kits” detect the presence of LH in urine and can detect a rise in this hormone that occurs one to two days before ovulation.In contrast to blood progesterone levels, urinary LH tests can predict ovulation before it occurs. Urinary LH testing helps define the times of greatest fertility: the day of the LH surge and the following two days. However, these tests can be expensive and should only be used by women with menstrual cycles that are consistently 25-35 days in length.
Sonohysterography
This procedure uses transvaginal ultrasound after filling the uterus with saline (a salt solution). This improves detection of intrauterine problems such as endometrial polyps and fibroids compared with using transvaginal ultrasonography alone. If an abnormality is seen, a hysteroscopy is typically done. This test is often done in place of HSG.
Hysteroscopy
This is a surgical procedure in which a lighted telescope-like instrument (hysteroscope) is passed through the cervix to view the inside of the uterus. Hysteroscopy can help diagnose and treat abnormalities inside the uterine cavity such as polyps, fibroids, and adhesions (scar tissue).
Laparoscopy
This is a surgical procedure in which a lighted telescope-like instrument (laparoscope) is inserted through the wall of the abdomen into the pelvic cavity. Laparoscopy is useful to evaluate the pelvic cavity for endometriosis, pelvic adhesions, and other abnormalities. Laparoscopy is not a first line option in the evaluation of a female patient. Because of its higher costs and potential surgical risk, it may be recommended depending on the results of other testing and a woman’s history, such as pelvic pain and previous surgeries.What is HSG Testing?
Though HSGs have been performed on women for over 100 years, it is arguable how much that test has advanced over that time.
Why an alternative to HSG testing was needed? “The fact is, fertility testing often takes too long and doesn't give clear answers," says Dr. Parry." We needed something that gave fast results without hurting and still was accurate and safe." The problem with the HSG test is it is often painful and not always conclusive.
Why the need for a new type of Fertility Test?
The problem with HSG Testing
As noted by Dr. Parry, HSG's can provide information, but often the insights are more limited than many realize.
A two dimensional black and white X-ray can miss details. The high pressure associated with many HSG’s not only can be painful, but also reflects a situation that sperm don’t really achieve. (Sperm don’t swim with the jaws of life to prop open an otherwise closed tube.) HSG’s also use radiation, can cause allergic reactions, and seem to have a higher rate of infection than ultrasound or office hysteroscopy. Furthermore, endometritis can’t be diagnosed with an HSG test.
Parryscope Fertility Testing approach provides a breakthrough in female fertility testing with multiple advantages over HSG testing. Dr. Parry’s innovation, including patents with the Parryscope® technique, can help you accurately, gently, and quickly understand factors in female fertility with a single office visit.

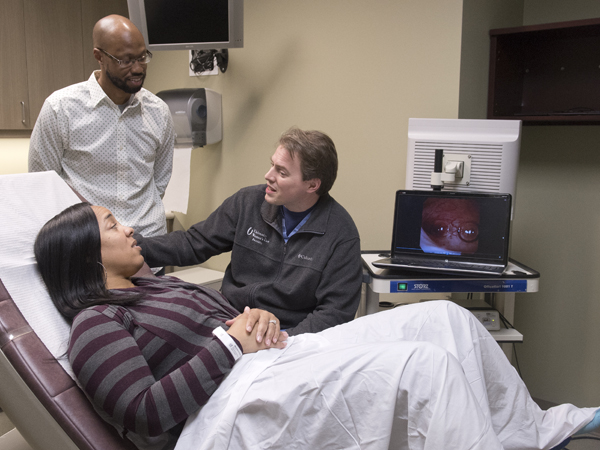
Dr. Preston Parry
Are there alternatives to HSG fertility testing? YES!

The Parryscope Fertility Testing approach provides a breakthrough in female fertility testing and more effective alternative to HSG Testing. The Parryscope® is a patented diagnostic device that can accurately, gently, and quickly reveal factors in female fertility with a single office visit. Not merely a piece of equipment, the Parryscope is a specific procedure that replaces HSG.
The Parryscope approach is Dr. Parry's breakthrough fast, effective and gentle testing method that evaluates the core aspects of female fertility – ovarian reserve, fallopian tube patency (meaning whether the tubes are open so sperm and egg can meet) and uterine factors – in a single diagnostic procedure.
Just as important as the test itself, Parryscope fertility testing includes our discussion of results in the same appointment, using easy-to-understand language that provides clear guidance on next steps.
What do Patients say about the Parryscope Fertility Testing Approach?
Ashley Maryland's two medical procedures done to figure out why she was having trouble becoming pregnant were like night and day.
"It was awful," Maryland, a Vicksburg resident, said of the HSG performed there in 2013. "It was overwhelming pain, and there was nothing I could do. It was the worst pain ever."
But her follow-up procedure with Dr. Parry was a completely different experience.
"I anticipated it hurting. I prepared myself for it. But it didn't hurt at all, and I got to watch it on a screen," Maryland said. "It was as lovely as it could be for that type procedure."
Source: umc.edu/news
How does the Parryscope Fertility Testing Approach work?
Dr. Parry’s procedure uses a narrow, flexible fiber-optic camera, saline, and air to determine if the saline and air bubbles can enter the fallopian tubes and if the uterus is receptive to pregnancy. Dye isn’t used at all.
“If the air bubbles don’t go in, the sperm may have trouble getting in, too.” says Dr Parry “We use technology so small and gentle that the speculum for a Pap smear is typically worse. The camera is the width of a coffee straw.”
An article published in 2017 showed that 91% of women undergoing Parryscope have mild to no discomfort, as opposed to 32% undergoing the HSG test reported extreme discomfort.
The goal of our test is to identify a woman’s chances for pregnancy quickly and to help her decide whether she should continue with natural conception, try oral medication and insemination, or move on to an assisted reproductive technology, such as in vitro fertilization (IVF) .

Patented breakthrough in Fertility Testing:
Less Pain. More Accurate.
The Parryscope Fertility Diagnostic Approach
20-minute procedure - three female infertility tests in one.
Fertility Factor #1: Are there a reasonable number of eggs?
To determine this, we use ultrasound to perform an antral follicle count (AFC) for the ovaries. Antral follicles are small sacs filled with fluid that contain an immature egg. We measure and count the antral follicles in both ovaries to determine whether the number of potential eggs remaining in the ovaries is low, normal or robust.
Fertility Factor #2: Can sperm and eggs meet in the fallopian tubes for fertilization?
Using Dr. Parry's unique Parryscope technique, we determine whether one or both fallopian tubes are blocked or damaged. Blocked or damaged fallopian tubes can affect pregnancy chances in two ways: by preventing sperm from reaching the egg for fertilization and/or preventing a fertilized egg from reaching the uterus for implantation. When combined with an ultrasound, the Parryscope can sometimes identify scarring in the pelvis that might reflect previous infection, endometriosis, or other problems.
Fertility Factor #3 Is the uterus favorable for embryo implantation and successful pregnancy?
Using ultrasound to understand the broader pelvis and outer uterus and a special thin and flexible hysteroscope for the inner uterus, we get valuable insight as to whether the uterus can accept and nurture the embryo.
The Parryscope technique is as safe if not safer than alternative approaches, with likely fewer infections (a less than .2% infection rate) and rare vasovagal events. And Parryscope is dramatically less painful to patients. Only 0.2% experienced maximum discomfort with the Parryscope technique, compared with 32% for HSG testing.
This is crucial, as many instances of infertility are due to a woman's fertilized egg failing to implant in the uterus for development. Issues with the uterus may also cause miscarriages after pregnancy (also known as recurrent pregnancy loss), which can be a problem distinct from infertility.
Top 10 reasons to choose Parryscope fertility testing
- Parryscope is fast, providing most women with what they need to know about their fertility in a 20-minute procedure.
- It is over 98% successful in identifying blockages.
- Parryscope is accurate.
- Parryscope is very gentle.
- Patients get immediate and precise fertility results to help with future decision-making.
- It is as safe - if not safer - than alternative approaches, with likely fewer infections (less than .2% infection rate) and vasovagal events.
- Cervical dilation, which can be painful, is less likely with the Parryscope approach, and reduces the risk for tubal spasm.
- Less Pain: Only 0.2% experienced maximum discomfort with the Parryscope technique, compared with 32% for HSG testing.
- Parryscope avoids radiation/X-rays, which can damage molecular structures and potentially jeopardize patient health.
- Parryscope uses air and saline, unlike HSG that can use dyes that result in allergic reactions. Research has shown severe cramping can result when the dye is administered in the traditional HSG x-ray fertility diagnostic approach.