As a fertility specialist, I’ve seen firsthand how deeply personal and challenging the journey to parenthood can be. Infertility affects about 15% of couples in the reproductive age group worldwide, according to the American Society for Reproductive Medicine (ASRM). According to the CDC, “In the United States, 1 in 5 (19%) of married women aged 15 to 49 with no prior births are unable to get pregnant after 1 year of trying. About 1 in 4 (26%) of women in this group have difficulty getting pregnant or carrying a pregnancy to term.”
Yet, despite how common it is, misconceptions about infertility often prevent couples from acknowledging their struggles. In fact, nearly half of those experiencing difficulty conceiving—48% according to a 2020 SingleCare survey—dismiss their challenges as something other than infertility.
This hesitation to seek help delays critical interventions and leaves many couples feeling isolated and uncertain about their next steps. In this post, I want to shed light on why so many couples avoid labeling their struggles as infertility, discuss the medical benchmarks for diagnosis, explore the roles male and female factors play, and address how confronting the stigma surrounding infertility can pave the way for earlier and more effective treatments.
What Defines Infertility? The Medical Benchmarks
The term infertility might sound intimidating, but its definition is straightforward. The American College of Obstetricians and Gynecologists (ACOG) defines infertility as the inability to conceive after 12 months of regular, unprotected intercourse for women under 35. For women over 35, the time frame shortens to six months due to the natural decline in fertility with age.
Importantly, this definition doesn’t assign blame. Infertility is a medical condition that affects both women and men, with approximately 40-50% of cases attributed to male factors, according to ASRM.
When to Seek Help
- Under 35: After 12 months of trying to conceive without success.
- 35 and Older: After six months of trying.
- Recommend Immediate Consultation: For those with known reproductive issues, irregular cycles, or a history of miscarriage.
Yet, many couples delay seeking help, often assuming that they just need more time or that stress or timing is the issue. This misunderstanding can have significant implications for their fertility journey. If you’ve been trying for a few months and still haven’t gotten pregnant, don’t worry just yet. The odds are still in your favor. About 75% of women who conceive will do so within three months, and almost 88% will do so within six months. But if it’s been 12 months or longer and you’ve had no luck, it’s probably time to see a fertility specialist.
Why Do So Many Couples Hesitate to Label Their Struggles as Infertility?
- Misconceptions About Infertility One of the primary reasons couples avoid the term infertility is a lack of awareness. Many believe infertility refers only to complete sterility or that it’s solely a woman’s issue. According to the ASRM, infertility encompasses a wide range of conditions, including hormonal imbalances, structural issues, and unexplained infertility, which affects up to 30% of couples.
- Stigma Surrounding the Term For some, the term infertility carries emotional weight. It may feel like a judgment or a label that diminishes their self-worth. Women, in particular, often internalize these feelings, associating infertility with personal failure. This stigma can make it difficult for couples to openly discuss their struggles, even with medical professionals.
- Lack of Understanding About Timing Couples often underestimate how long it should take to conceive naturally. The Journal of Reproductive Medicine notes that while some couples conceive within the first three months of trying, up to 20% may take a year or longer. This natural variability can create confusion, leading some to dismiss their struggles as normal, even when medical intervention might be beneficial.
- Emotional Avoidance The fear of receiving a formal diagnosis of infertility can lead couples to avoid seeking help altogether. Facing the possibility of needing medical intervention can be overwhelming, particularly when associated with financial or emotional stress.
The Role of Male Factor Infertility
One of the most overlooked aspects of infertility is the significant role male factors play. According to the American College of Obstetricians and Gynecologists (ACOG), male infertility contributes to nearly half of all infertility cases. Conditions such as low sperm count, poor motility (the ability of sperm to move effectively), abnormal morphology (the shape and structure of sperm), and hormonal imbalances can all impact a couple’s ability to conceive. Additionally, lifestyle factors such as smoking, alcohol use, obesity, and even prolonged exposure to environmental toxins can exacerbate these issues.
Why Male Testing Matters
Despite these statistics, male testing is often delayed or overlooked entirely. Cultural stigmas, assumptions that fertility challenges lie solely with the woman, or simply a lack of awareness about male infertility can all contribute to this delay. Unfortunately, this misconception not only postpones effective diagnosis and treatment but can also place an undue emotional and physical burden on the woman, who may undergo unnecessary invasive procedures while the true underlying issue remains unaddressed. By prioritizing a comprehensive evaluation that includes both partners early in the process, couples can save valuable time and avoid added stress.
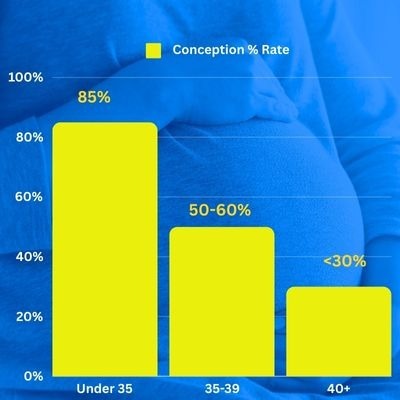
The Impact of Delaying Fertility Evaluation
“There’s no need to face your fertility challenges in isolation,” I often tell patients. “Answers and support are just a phone call away.” Yet, so many couples delay seeking help, unsure if their struggles are serious enough to warrant attention. This hesitation can have real consequences. Fertility naturally declines with age, particularly for women. By the mid-30s, egg quantity and quality drop significantly, as highlighted by the American Journal of Obstetrics and Gynecology. For men, sperm quality also diminishes over time, making early evaluation equally important for both partners.
I’ve seen the transformation that happens during a first consultation. Couples often arrive with apprehension—elevated blood pressure, racing hearts—but leave with relief and optimism. Why? Because knowledge empowers. Understanding your fertility gives you control, clarity, and actionable steps forward.
Delaying evaluation can limit your options. Early testing can reveal correctable issues, open doors to less invasive treatments, and improve your chances of conceiving. Whether it’s a hormone imbalance, lifestyle factors, or a more complex condition, addressing it now gives you the best chance for success.
Conception Rates Over Time
- Under 35: 85% conceive within one year.
- 35-39: 50-60% conceive within one year.
- 40 and older: Less than 30% conceive within one year.
Redefining Infertility: A Medical, Not Personal, Diagnosis
One of the most empowering shifts couples can make is to view infertility as a neutral medical condition, not a reflection of personal inadequacy. Infertility is not about failure or blame; it’s a health issue, much like diabetes or hypertension. By reframing it in this way, couples can reduce the emotional burden and focus on actionable steps toward resolution.
This perspective shift is crucial because infertility often carries an unjust stigma, fueled by societal pressures and misconceptions. For many, the inability to conceive feels deeply personal, leading to feelings of guilt, shame, or even isolation. But the truth is, infertility is a medical diagnosis that affects millions of couples worldwide, with identifiable causes ranging from hormonal imbalances and structural issues to lifestyle factors and genetics.
Understanding this can help couples approach their fertility journey with a more balanced mindset. Just as you wouldn’t hesitate to seek treatment for a broken bone or high blood pressure, seeking help for infertility is a proactive step toward restoring health and achieving your family goals. The sooner couples embrace this perspective, the sooner they can take advantage of the many diagnostic and treatment options available to them, transforming uncertainty into hope.
Taking the First Step: A Checklist for Couples
For couples unsure whether to seek help, this simple checklist can provide clarity:
- Track Timing: Have you been trying to conceive for 12 months (under 35) or 6 months (35 and older) without success?
- Evaluate Cycles: Are menstrual cycles irregular or absent?
- Consider History: Do you or your partner have a history of reproductive health issues, such as PCOS, endometriosis, or low sperm count?
- Assess Age: Are you over 35 and looking to conceive for the first time?
- Check Symptoms: Are there signs of hormonal imbalance, such as weight changes, acne, or hair loss?
If you answered yes to any of these questions, it may be time to consult a fertility specialist.
How Positive Steps Fertility Can Help
At Positive Steps Fertility, we understand how overwhelming the infertility journey can be. That’s why we’ve made it our mission to provide innovative, compassionate, and effective care tailored to your unique needs. Our breakthrough approach, developed by Dr. John Preston Parry, is revolutionizing fertility diagnostics and empowering women with answers faster than ever before.
Introducing the 20-Minute Fertility Test
Dr. Parry’s patented 20-Minute Fertility Test is a game-changer for women seeking clarity about their fertility. This device and technique are designed to minimize discomfort while providing a faster, safer, and more affordable solution to fertility testing.
Here’s what makes it exceptional:
- Comprehensive Evaluation: The test evaluates the three critical factors in female fertility:
- Ovarian Egg Reserve: Determines the quantity and quality of a woman’s remaining eggs.
- Fallopian Tube Blockage: Assesses whether the tubes are open for the egg and sperm to meet.
- Uterine Health: Examines the uterus’s suitability for embryo implantation and a successful pregnancy.
- Same-Day Results: In just one office visit, patients receive a clear and in-depth understanding of their fertility, explained in simple, actionable terms.
- Minimized Discomfort: Unlike traditional methods, this diagnostic approach is gentle, prioritizing the patient’s comfort and emotional well-being.
- Efficiency and Cost-Effectiveness: Faster and less expensive than conventional tests, the 20-Minute Fertility Test makes accurate fertility evaluation more accessible to everyone.
Once the 20-Minute Fertility Test identifies the root causes of infertility, Dr. Parry and his team create a personalized treatment plan. Whether the next steps involve lifestyle adjustments, medication, or advanced fertility treatments like IUI or IVF, patients leave with clarity and confidence about their path forward.
Empowering Couples to Seek Help
Infertility doesn’t have to be a lonely or shameful journey. By recognizing the medical nature of infertility and addressing the misconceptions surrounding it, couples can take the first step toward finding solutions and building their families.
If you’ve been struggling to conceive, don’t wait. Reach out to a trusted fertility clinic to learn more about your options. With the right support and resources, hope is always within reach.
Don’t suffer in silence. Get answers. Get peace. Your journey to parenthood starts with a conversation, and we’re here to guide you every step of the way.