The relationship between age and fertility is multifaceted. For many, age doesn’t immediately present a barrier to conception. In fact, numerous women who choose to conceive later in life, often for the first time, find success without significant difficulties.
However, as a woman ages, the odds of conception generally decrease. For context, 75% of women can typically expect to conceive within three months of discontinuing contraception. The age factor becomes even more pronounced for those who have waited a prolonged duration, be it 2, 3, or even 10 years, to start their journey towards parenthood. These delays can sometimes compound the challenges tied to age-related fertility.
Here’s a closer look at the impact of age on egg quality:
- At the age of 25, a vast majority of a woman’s eggs, around 80-90%, are chromosomally normal.
- However, by the time a woman reaches 40, approximately three-fourths of her eggs are chromosomally abnormal, which means that during the span of a year, only about three months offer a fair chance of conception with a chromosomally normal egg.
This decreasing ratio of healthy eggs to abnormal ones as age advances justifies the often aggressive medical interventions recommended for older women trying to conceive. A 40-year-old will need three or four eggs to find just one chromosomally “normal” egg. As a result, even with medical intervention, the risk of multiple pregnancies is typically reduced in older women.
While age undeniably plays a significant role in fertility, it isn’t an insurmountable hurdle. With the right guidance, support, and possible medical assistance, many women can realize their dream of motherhood at various stages of life.
How Does Age Impact Fertility and Pregnancy Health?
Age plays a dual role when evaluating fertility and the health of a pregnancy:
- Conception Rates : The probability of getting pregnant varies significantly with age. A 40-year-old who’s been trying for a year might have only a 1% chance of conception per month. In contrast, a 25-year-old in a similar situation might have a 4% monthly chance. Thus, age is a factor, but the duration of one’s conception journey also plays a pivotal role.
- Pregnancy Health : As age increases, so do potential complications during pregnancy. For example:
- By the age of 40, the miscarriage rate can soar to 40% or even higher, contingent on the duration of one’s conception efforts.
- The risk of chromosomal abnormalities, such as Down syndrome, also escalates. A 40-year-old might face odds of 1 in 100 or even 1 in 50 for giving birth to a child with Down syndrome.
These increasing challenges highlight the importance of not just seeking support to conceive, but also undergoing thorough medical evaluations during pregnancy. If you’re considering parenthood later in life, it’s imperative to maintain close coordination with a fertility specialist to ensure the best outcomes for both mother and child.
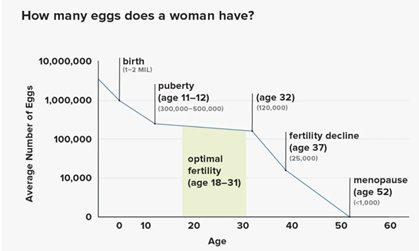
How Do My Eggs Change Over Time?
Eggs undergo changes as we age, both in quantity and quality.
According to the American College of Obstetricians and Gynaecologists (ACOG), a female fetus typically has around 6–7 million eggs at 20 weeks of gestation, dropping to 1–2 million at birth.
A common misconception is that women lose one egg per month. In reality, about 900 eggs are lost each month, roughly 30 eggs daily. Even with high-end fertility medications, fertility specialists can retrieve only a certain number of these eggs:
- At age 30, you can typically retrieve around 25 eggs.
- By 35, this number drops to an average of 16 eggs.
- At 40, you might be able to retrieve around 8 eggs.
This downward trend in retrievable eggs over time demonstrates the importance of time when considering fertility treatments.
However, it’s not just about the number of eggs. Quality is equally crucial. A 30-year-old woman generally has around 75% of her eggs chromosomally normal. By 35, this drops to approximately 50%; at age 40, it’s about 25%. In summary, as we age, both our eggs’ quantity and quality decline.
Egg quality and quantity can vary significantly among women. For instance, my wife and I discovered that at 41, she had fewer eggs than average for her age when we were trying to conceive our son, Lucas. Fortunately, the eggs’ quality was superb. Your physician needs to assess the number of viable eggs. Still, quality often reveals itself through a successful pregnancy or, in some cases, by combining IVF with PGT to biopsy the embryo’s DNA.
How does my age influence potential complications during pregnancy?
As women age, the likelihood of encountering pregnancy complications increases. Such complications can include the development of fibroids, which are growths in the uterine muscle, and polyps, which form in the uterine lining.
Over time, there’s also a risk of accumulating infections and other health issues. Beyond these factors, the physical process of pregnancy can become more challenging due to various reasons, such as weight gain or the onset of medical conditions like high blood pressure and diabetes. These conditions can result in premature births, preterm labor, or preeclampsia, a condition akin to an allergic reaction to pregnancy affecting blood pressure and protein processing in the body, leading to swelling.
All these factors underscore the importance of close coordination with your obstetrician and fertility specialist. If you have multiple medical conditions, consulting a maternal-fetal medicine specialist might also be beneficial. This expert has general obstetrics training but specializes in managing high-risk pregnancies.
At What Age Do Women Typically Run Out of Eggs?
It’s a great question. I’ll default to our go-to answer in medicine: it depends.
For women, understanding egg count is best visualized as a continuum. Remarkably, some women in the lowest 5% for egg count at birth might have a similar number of eggs as those in the top 5% when they reach 40. Given this vast variation, individual evaluations are essential. Remember, eggs’ quantity and quality change as women age.
For context, some women born with a lower egg count may have the same number of eggs at birth as others at 40. So, it’s crucial to understand that egg count and fertility are on a spectrum and should be evaluated individually.
An interesting study to consider involves the Hutterites, a Christian sect settled across the agricultural colonies of the Great Plains in the U.S., including Montana and North Dakota. Living without contraception and having minimal exposure to STDs due to their isolated communities, they offer a unique perspective on fertility. Remarkably, even among these highly fertile women, who on average bear eight children, half struggle to conceive past the age of 40. This observation underscores the reality that time can impact even the most fertile individuals.
So, I think everyone should be mindful of the biological clock ticking. Women in their mid to late 20s to early 30s generally have a healthy egg reserve. However, if you are wondering why conception hasn’t occurred, it may be worth seeking a fertility evaluation.
As women approach and move through their late 30s, fertility can decline to a rate of about 20% per year or around 1.5% per month. This decline can accelerate in the 40s to about 2.5% per month, or 30% per year, making it imperative to be proactive about reproductive health.
Why does fertility decline as you get older?
This is a great question, as it affects so many women. It’s an inquiry many women have, and there’s a scientific reason behind it. Primarily, women tend to ovulate their highest quality eggs first, adhering to what’s called the production line theory. Imagine a game of telephone; when you’re just a couple of players in, the message remains clear. But when you’re 20 players in, the original message becomes distorted.
At the ages of 20-25, most eggs released possess normal DNA. However, as time progresses and age increases, the eggs released are often “later-generation” copies. This extended replication increases the chances of errors, leading to issues like extra or missing DNA, which can result in miscarriages or congenital disabilities.
Interestingly, this phenomenon predominantly impacts women. While men are affected, too, the errors in their reproductive cells manifest differently.
Think of fertility like a book. As women age, it’s analogous to missing a chapter, page, or paragraph, given that they are born with all the eggs they’ll ever have.
In contrast to women, men continuously produce new sperm daily. This ongoing production can lead to minor genetic errors, analogous to a missing sentence, or word, or letter in a book. These small genetic discrepancies are referred to as point mutations. Such minuscule mistakes in sperm are more challenging to detect. When using PGT, a procedure involving IVF where embryos are biopsied to identify abnormalities, it’s typically easier to spot errors originating from the egg than those from the sperm.
Final Thoughts: Age and Fertility Are Factors, But Not a Final Verdict
Fertility and age are closely connected, but age is never the only deciding factor. While egg quality and quantity naturally decline over time, many women still conceive later in life—sometimes naturally, sometimes with the help of fertility treatment. The key is not just watching the clock, but understanding where you stand right now. Every woman’s fertility journey is unique, and the best path forward depends on clear answers, not assumptions.
Next Steps You Can Take
At Positive Steps Fertility, we’re here to provide clarity and support as you navigate this journey. If you’re feeling frustrated or unsure about your next steps, let us help.
My goal is to provide women with clear, evidence-based answers so they can make informed decisions. Together, we can identify what’s truly impacting your ability to conceive and develop a plan to address it. You don’t have to go through this alone. Reach out today and take the next positive step forward.
Do you still have questions?
- Learn more: Recognizing and Treating DOR
- Watch my YouTube Video on Age and Fertility
- Sign up for our 20-minute fertility diagnostic test, the Parryscope Test, invented by Dr. Parry.
If you’re ready for answers now, schedule a consultation with our team. Don’t suffer in silence. Find answers. Find peace. Reach out today.




