Diagnosing infertility depends on the source of the problem. One of the main factors for fertility is whether the fallopian tubes are open. Women are born with two fallopian tubes, each connecting the ovary to the uterus. When one or both are blocked, infertility can result.
A blocked fallopian tube can prevent the sperm from reaching the egg or keep the fertilized egg from implanting in the uterus. Instead, a damaged tube can lead to an ectopic pregnancy, where the embryo sticks in the tube instead of implanting in the uterus. It is always fatal for the fetus and can sometimes be life-threatening for the mother.
HSG has been the standard fertility test for the last hundred years.
The HSG Test was first described in 1911 and has since been the standard infertility test for determining whether the fallopian tubes are open. But it’s arguable how much the HSG test has advanced over time.
What is HSG Testing?
According to the American College of Obstetricians and Gynecologists, “Hysterosalpingography (HSG) is an X-ray procedure used to view the inside of the uterus and fallopian tubes.
- HSG often is used to see if the fallopian tubes are partly or fully blocked.
- It also can show if the inside of the uterine cavity is of normal size and shape.
- All of these problems can lead to infertility and pregnancy problems.
Why is there a need for an HSG alternative?
HSG testing can provide some valuable information to a fertility specialist, but the insights are often more limited than many realize.
A two-dimensional black and white X-ray can miss details. Additionally, the high pressure associated with many HSG tests can be painful and reflect a situation that sperm don’t really achieve.
“Unlike the pressure used in HSG testing, sperm don’t swim with the ‘jaws-of-life’ to prop open an otherwise closed fallopian tube.” Dr. Preston Parry
HSGs also use radiation, can cause allergic reactions, and seem to have a higher infection rate than ultrasound or office hysteroscopy. Furthermore, endometritis can’t be diagnosed with an HSG test.
In short, the HSG fertility test for women is often painful and not always conclusive.
“The fact is, fertility testing often takes too long and doesn’t give clear answers,” says Dr. Parry. “We needed something that gives fast results without hurting and is still accurate and safe.”
The Parryscope Fertility Test: a better approach to understanding the Fallopian tubes
The Parryscope® technique is a breakthrough approach to fertility testing that can accurately, gently, and quickly evaluate the core aspects of female fertility with a single office visit.
Dr. Parry’s procedure uses a narrow, flexible fiber-optic camera, saline, and air to determine whether tiny air bubbles can enter the fallopian tubes and if the uterus is receptive to pregnancy. Unlike HSG testing, dye isn’t used at all.
“While looking in the uterus, we release air bubbles that travel to and through the fallopian tubes. If the air bubbles don’t go in, the sperm may have trouble getting in, too,” says Dr Parry “We use technology so small and gentle that the speculum for a Pap smear is typically worse. The camera is so tiny it is the width of a coffee straw.”
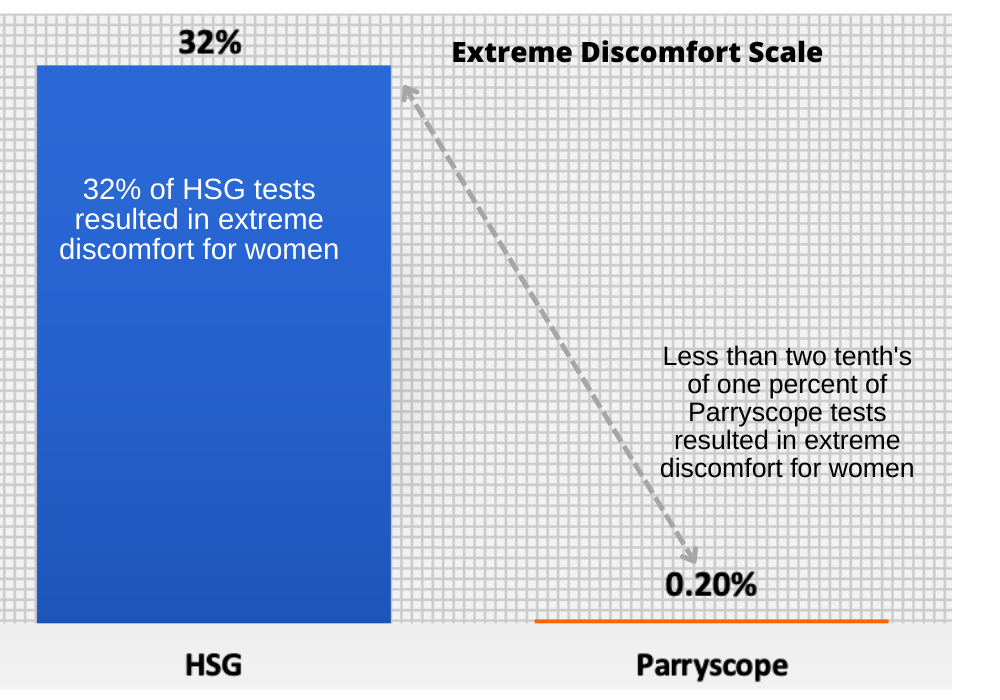
An article published in 2017 showed that women undergoing Parryscope testing had way less discomfort than the HSG approach.
- Parryscope® users: 91% reported having only mild to no discomfort and only 0.2% had extreme discomfort.
- HSG users: 32% reported the HSG test caused extreme discomfort.
What’s Unique About the Parryscope Fertility Approach?
The Parryscope approach is groundbreaking for female fertility testing that replaces HSG and provides additional insight. It’s a fast, effective, and gentle testing method that evaluates three core factors in a woman’s fertility:
- Ovarian egg reserve,
- Are the Fallopian tubes open (Tubal Patency) to determine if there are any blockages that would keep sperm and egg from meeting, and the finally,
- Uterine receptivity for embryo implantation and successful pregnancy.
The Parryscope procedure is a 15-minute test that provides immediate results with easy-to-understand language and perspective. Each woman walks away with a clear insight into the core factors for her infertility and the most likely treatment options for pregnancy.
The Parryscope® approach evaluates 3 core fertility factors in a single test.
Number 1. Parrycope fertility testing answers if there are a reasonable number of eggs?
We use ultrasound to perform an antral follicle count (AFC) for the ovaries to determine this. Antral follicles are small sacs filled with fluid that contain an immature egg. We measure and count the antral follicles in both ovaries to determine whether the number of potential eggs remaining in the ovaries is low, normal, or robust.
Number 2. Parryscope testing shows if sperm and eggs can meet in the fallopian tubes for fertilization?
Using Dr. Parry’s unique Parryscope technique, we determine whether one or both fallopian tubes are likely to be blocked or damaged. Blocked or damaged fallopian tubes can affect pregnancy chances in two ways:
- By preventing sperm from reaching the egg for fertilization;
- By hindering a fertilized egg from reaching the uterus for implantation.
When combined with an ultrasound, the Parryscope can sometimes identify scarring in the pelvis that might reflect previous infection, endometriosis, or other problems.
Number 3. Parryscope will examine if the uterus is favorable for embryo implantation and successful pregnancy?
The Parryscope technique is as safe – if not safer – than alternative approaches, with likely fewer infections (a less than .2% infection rate) and rare vasovagal events.
Parryscope is also dramatically less painful to patients compared to HSG. Only 0.2% experienced maximum discomfort with the Parryscope technique, compared with 32% for HSG testing.
Combining ultrasound to examine the broader pelvis with a special thin and flexible hysteroscope for the inner uterus, Parryscope provides valuable insight into whether the uterus can accept and nurture the embryo.
Evaluating the uterus is crucial, as infertility is often due to a woman’s embryos failing to implant in the womb. Issues with the uterus may also cause miscarriages.
It’s time to replace the 100-year-old HSG fertility test.
If you could have a fertility test that’s more accurate, gentler, cheaper, and faster, wouldn’t you do it? Welcome to a whole new way to diagnose infertility, The Parryscope Approach.




